Authors
- Fisher*,1 S. Selvin,2 G. V. Heller,2 S. Curran,1 T. Mathur,1 L. Immordino,1 S. Chandhok,1 F. Day,1 J. Hazel-Dabagian,1 J. Steers,1 G. Harper,1 L. Mendelson,1 H. Kramer,1 S. Mangalmurti1; 1Bryn Mawr Hospital, Lankenau Heart Institute, Bryn Mawr, PA, 2Molecular Imaging Services, Newark, DE
Abstract
Background: Cardiac PET myocardial perfusion imaging (MPI) is now being implemented in many clinical nuclear cardiology laboratories throughout the United States because of higher diagnostic accuracy, better image quality and lower radiation exposure, which should change post-test referral patterns. The purpose of this study was to examine the outcomes of a similar population of Medicare patients from the same cardiology group who underwent either SPECT or PET MPI. The outcome measures were cardiac catheterization and revascularizations following either testing procedure.
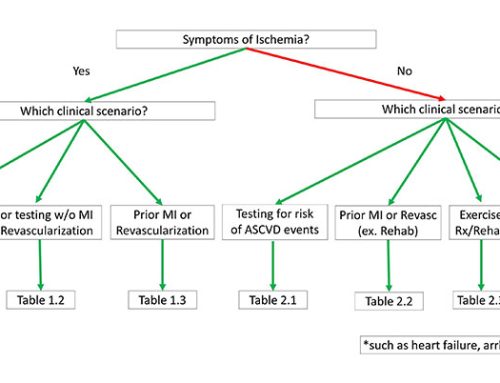
Methods: Consecutive Medicare patients who met AUC criteria and underwent SPECT or PET MPI were followed as to whether they underwent cardiac catheterization and intervention within 60 days of the nuclear procedure. The percentage of normal results at catheterization from each group was also determined.
Results: 1328 SPECT patients in 9 months preceding the PET program were evaluated (mean age 76.5), and compared to 703 PET patients for 6 months after program initiation (mean age 75.7). Cardiac catheterization was performed in 6.9% of SPECT MPI and 6.1% of PET MPI (11.7% reduction, p=NS). For those patients who underwent catheterization, intervention (either PCI or CABG) was performed in 43.5% of SPECT patients and a higher percentage for PET MPI, 53.5% (p=NS). Of SPECT MPI patients, 41.3% were found to have no or insignificant CAD at catheterization compared with 16.3% of PET patients (p<0.001))
Conclusion: Cardiac PET MPI should affect downstream testing. We found initiation of cardiac PET myocardial perfusion imaging into a clinical cardiology practice resulted in a reduction of the number of patients referred for cardiac catheterization as well as significantly fewer unnecessary catheterizations (normal) and a higher percentage of interventions.